EMR systems for home health are revolutionizing how healthcare is delivered in the home setting. These systems offer a comprehensive suite of tools that streamline patient care, enhance communication, and boost operational efficiency. From managing patient demographics and clinical documentation to scheduling appointments and automating billing processes, EMR systems empower home health agencies to provide high-quality care while navigating the complexities of modern healthcare.
The integration of telehealth capabilities further elevates the role of EMR systems in home health. Remote patient monitoring and virtual consultations enable healthcare providers to stay connected with patients, ensuring continuity of care and facilitating proactive interventions. This, in turn, contributes to improved patient outcomes and a more personalized care experience.
Introduction to EMR Systems in Home Health: Emr Systems For Home Health
The evolution of Electronic Medical Records (EMR) systems in home health has been driven by a confluence of factors, including the increasing complexity of patient care, the need for enhanced efficiency, and the growing emphasis on regulatory compliance. The adoption of EMR systems has transformed the way home health agencies operate, bringing about significant advancements in patient care, operational efficiency, and regulatory compliance.
Benefits of Implementing EMR Systems in Home Health Agencies
EMR systems have revolutionized home health care by providing numerous benefits that enhance patient care, improve operational efficiency, and ensure regulatory compliance. The adoption of EMR systems has transformed the way home health agencies operate, leading to improved patient outcomes and streamlined workflows.
- Improved Patient Care: EMR systems enable comprehensive patient data management, facilitating better informed clinical decision-making. The electronic storage and retrieval of patient information allows for a holistic view of the patient’s medical history, enabling healthcare providers to deliver personalized and tailored care. The integration of clinical guidelines and best practices within EMR systems ensures that care plans are evidence-based and meet the specific needs of each patient.
Moreover, EMR systems enable real-time monitoring of patient progress, allowing for timely interventions and adjustments to care plans. This proactive approach to patient care leads to improved outcomes, reduced hospital readmissions, and enhanced patient satisfaction.
- Operational Efficiency: EMR systems streamline administrative tasks, reducing paperwork and improving operational efficiency. Automated scheduling, billing, and reporting functions eliminate manual processes, freeing up valuable time for healthcare professionals to focus on patient care. The centralized repository of patient data enables seamless communication among healthcare providers, improving coordination of care and reducing redundancies. Furthermore, EMR systems facilitate data analysis and reporting, providing insights into agency performance and identifying areas for improvement.
- Regulatory Compliance: EMR systems ensure compliance with evolving regulations and standards. The electronic documentation and tracking capabilities of EMR systems meet the requirements of regulatory bodies such as Medicare and Medicaid, minimizing the risk of penalties and sanctions. The integration of clinical guidelines and best practices within EMR systems ensures that care plans adhere to established standards, promoting patient safety and quality care.
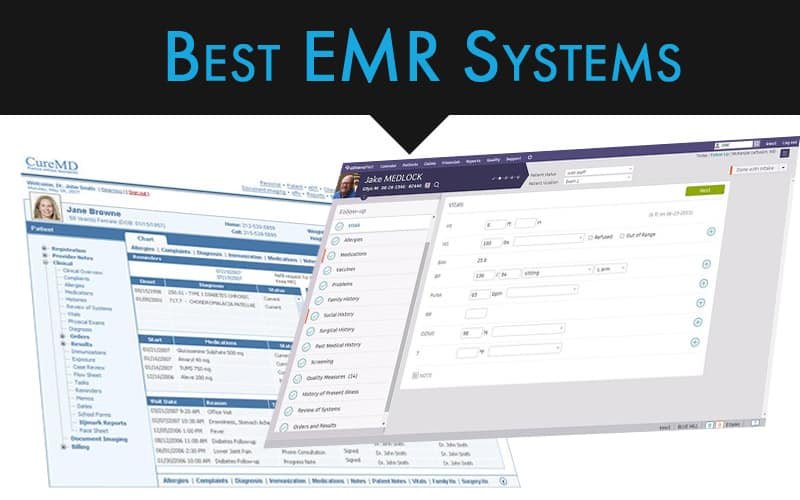
Types of EMR Systems Available for Home Health Agencies
A diverse range of EMR systems cater to the specific needs of home health agencies, offering varying functionalities and features. The choice of EMR system depends on factors such as agency size, budget, and specific requirements.
- Standalone EMR Systems: These systems operate independently and are typically used by smaller home health agencies. They offer basic functionalities such as patient charting, scheduling, and billing. Standalone EMR systems are often more affordable than integrated systems but may lack advanced features such as data analytics and interoperability.
- Integrated EMR Systems: These systems integrate with other healthcare applications, such as billing software and patient portals. Integrated EMR systems offer comprehensive functionalities, including patient charting, scheduling, billing, and data analytics. They are typically used by larger home health agencies and provide a more holistic view of patient care.
- Cloud-Based EMR Systems: These systems are hosted on a cloud platform, providing access from any device with an internet connection. Cloud-based EMR systems offer scalability, affordability, and ease of use. They are ideal for agencies that require flexibility and remote access to patient data.
Key Features of EMR Systems for Home Health

EMR systems specifically designed for home health agencies offer a comprehensive suite of features to streamline operations, enhance patient care, and improve overall efficiency. These systems cater to the unique needs of home health providers, incorporating functionalities that address patient demographics, clinical documentation, medication management, scheduling, and billing.
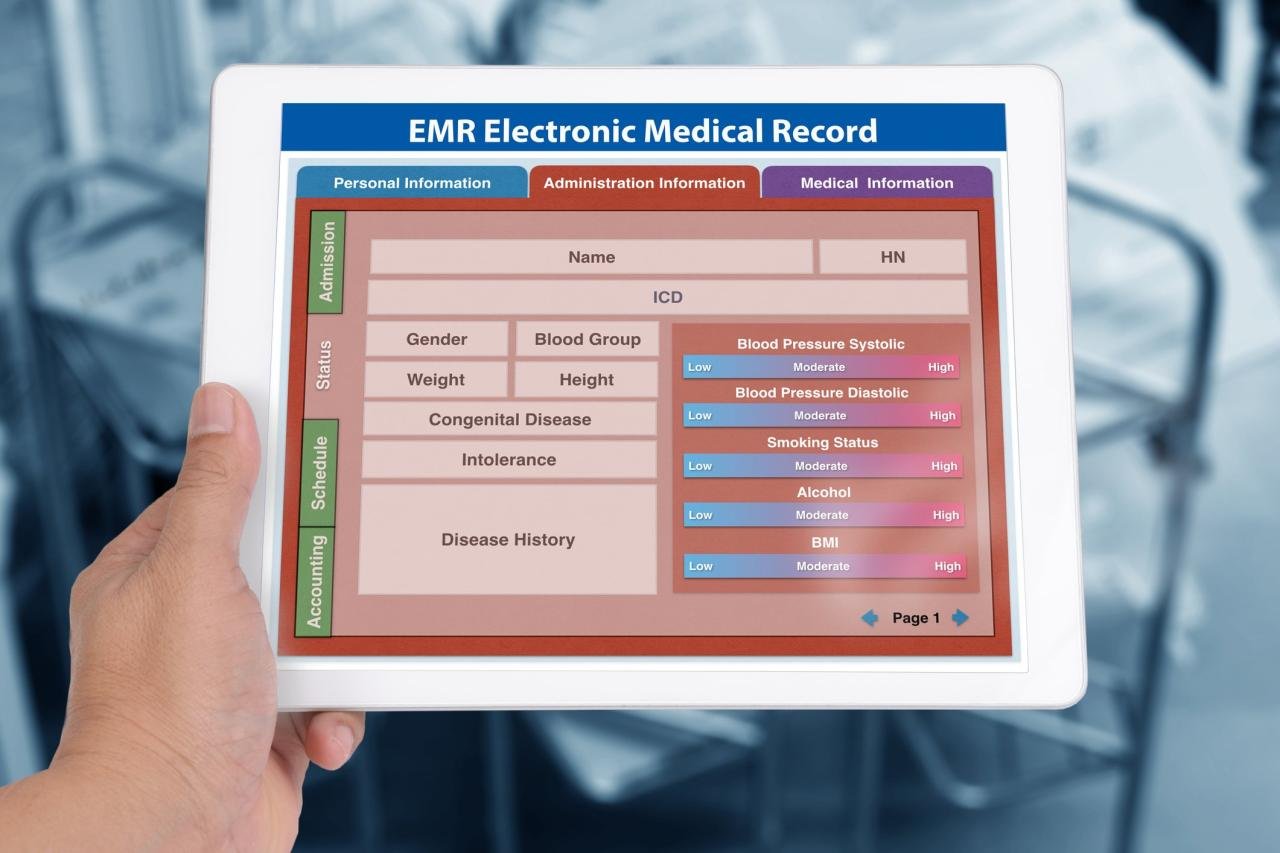
Patient Demographics
Patient demographics play a crucial role in personalized care. EMR systems in home health facilitate the capture and management of essential patient information, including:
- Personal details: Name, address, contact information, date of birth, gender, and insurance information.
- Medical history: Past diagnoses, surgeries, allergies, medications, and family medical history.
- Social determinants of health: Socioeconomic factors, lifestyle habits, and environmental influences impacting patient health.
This information helps home health providers understand patients’ unique needs and develop tailored care plans.
Clinical Documentation
Clinical documentation is the backbone of home health care. EMR systems provide a secure platform for recording, managing, and accessing patient medical records. Key features include:
- Electronic visit notes: Real-time documentation of patient visits, including assessments, interventions, and patient progress.
- Care plans: Development and management of individualized care plans, outlining goals, interventions, and frequency of visits.
- Progress notes: Tracking patient progress over time, highlighting changes in condition, response to treatment, and any complications.
- Medication management: Recording and monitoring patient medications, including dosages, frequencies, and potential interactions.
- Integrated communication tools: Secure messaging platforms for seamless communication between caregivers, patients, and families.
These features ensure comprehensive and accurate documentation, facilitating effective care coordination and communication among all stakeholders.
Scheduling and Billing
Efficient scheduling and billing are critical for home health agencies. EMR systems streamline these processes by:
- Scheduling appointments: Automated scheduling tools that consider patient availability, caregiver availability, and service needs.
- Route optimization: Algorithms that optimize caregiver routes, minimizing travel time and maximizing efficiency.
- Automated billing: Generating accurate and timely invoices, reducing manual errors and improving cash flow.
- Claims management: Tracking and managing insurance claims, ensuring timely reimbursement and reducing administrative burden.
By automating these processes, EMR systems free up valuable time for clinicians to focus on patient care.
Telehealth Integration
Telehealth integration has revolutionized home health care, enabling remote patient monitoring and virtual consultations. EMR systems with telehealth capabilities provide:
- Remote patient monitoring: Secure platforms for transmitting patient vital signs, such as blood pressure, heart rate, and blood glucose levels, directly to caregivers.
- Virtual consultations: Secure video conferencing tools for virtual consultations with patients, allowing for real-time assessments and follow-up care.
- Medication reminders: Automated reminders for patients to take their medications, improving adherence and reducing medication errors.
Telehealth integration enhances patient care by providing continuous monitoring, reducing hospital readmissions, and improving patient satisfaction.
Data Security and Privacy
Data security and privacy are paramount in home health EMR systems. These systems are designed to comply with regulations such as HIPAA (Health Insurance Portability and Accountability Act) and GDPR (General Data Protection Regulation). Key features include:
- Data encryption: Encrypting sensitive patient data to prevent unauthorized access.
- Access controls: Limiting access to patient information based on user roles and permissions.
- Auditing trails: Recording all user activity within the system to ensure accountability and identify potential breaches.
- Regular security updates: Implementing security patches and updates to address vulnerabilities and mitigate risks.
By prioritizing data security and privacy, EMR systems ensure the confidentiality and integrity of patient information, fostering trust and confidence in the healthcare system.
Benefits of Implementing EMR Systems in Home Health
EMR systems offer numerous advantages for home health agencies, leading to improved patient care, enhanced operational efficiency, and streamlined compliance efforts. By digitizing patient records, automating tasks, and facilitating communication, EMR systems empower home health professionals to provide more effective and efficient care.
Improved Patient Care
EMR systems play a crucial role in enhancing patient care by improving communication, reducing medication errors, and fostering better care coordination.
- Enhanced Communication: EMR systems facilitate seamless communication between healthcare providers, patients, and their families. Real-time access to patient records allows nurses, doctors, and other healthcare professionals to stay informed about a patient’s condition, treatment plan, and progress. This ensures consistent care and avoids duplication of efforts. For example, a home health nurse can access a patient’s medication list and allergies directly from the EMR system, ensuring accurate medication administration and minimizing the risk of adverse drug events.
- Reduced Medication Errors: EMR systems help reduce medication errors by providing comprehensive medication lists, automated alerts for potential drug interactions, and reminders for medication refills. By eliminating manual data entry and providing real-time information, EMR systems minimize the risk of human error, improving patient safety. For instance, a home health agency using an EMR system can set up alerts to notify nurses when a patient’s medication dosage needs to be adjusted based on their latest lab results.
This ensures appropriate medication management and prevents potential complications.
- Enhanced Care Coordination: EMR systems streamline care coordination by providing a central repository for patient information. This allows healthcare professionals to access and share information seamlessly, ensuring a holistic approach to patient care. For example, a home health agency can use an EMR system to track patient progress, communicate with other healthcare providers involved in the patient’s care, and schedule follow-up appointments.
This coordinated approach ensures that patients receive timely and appropriate care throughout their treatment journey.
Operational Efficiency
EMR systems significantly enhance operational efficiency by streamlining workflows, automating tasks, and improving billing accuracy.
- Streamlined Workflows: EMR systems automate many administrative tasks, such as scheduling appointments, generating reports, and managing patient records. This frees up valuable time for healthcare professionals to focus on providing direct patient care. For instance, an EMR system can automatically generate patient visit summaries, eliminating the need for manual documentation and saving nurses valuable time.
- Automated Tasks: EMR systems can automate repetitive tasks, such as data entry, appointment scheduling, and medication refills. This reduces the risk of human error and increases productivity. For example, an EMR system can automatically send appointment reminders to patients, reducing the number of missed appointments and improving patient engagement.
- Improved Billing Accuracy: EMR systems improve billing accuracy by automating the billing process and ensuring that all claims are submitted correctly. This reduces the risk of claim denials and improves revenue cycle management. For example, an EMR system can automatically generate invoices based on patient visits and services provided, reducing the risk of errors and improving billing efficiency.
Regulatory Compliance
EMR systems help home health agencies achieve regulatory compliance by providing tools for documentation, reporting, and data analysis.
- Documentation: EMR systems provide a secure and auditable platform for documenting patient care, ensuring compliance with regulations set by Medicare, Medicaid, and other relevant organizations. For example, an EMR system can track patient progress notes, medication administration records, and other essential documentation required for home health care. This ensures accurate and timely documentation, reducing the risk of audit findings and penalties.
- Reporting: EMR systems generate reports that meet regulatory requirements, such as quality assurance reports, outcome measures, and patient satisfaction surveys. This provides valuable data for performance improvement initiatives and ensures compliance with reporting obligations. For example, an EMR system can generate reports on patient falls, medication errors, and other quality indicators required by Medicare and Medicaid.
- Data Analysis: EMR systems provide tools for data analysis, allowing home health agencies to identify trends and patterns in patient care. This information can be used to improve care delivery, enhance patient outcomes, and ensure compliance with regulatory requirements. For example, an EMR system can analyze patient data to identify risk factors for hospital readmissions, allowing home health agencies to implement interventions to reduce readmission rates.
Choosing the Right EMR System for Home Health
Selecting the right EMR system for your home health agency is a crucial decision that can significantly impact your agency’s efficiency, patient care, and overall success. It requires careful consideration of your agency’s unique needs, budget, and long-term goals.
Factors to Consider When Selecting an EMR System, Emr systems for home health
Choosing the right EMR system for your home health agency involves evaluating various factors to ensure a seamless implementation and optimal utilization. Here’s a checklist to guide your decision-making process:
- Agency Size: The size of your agency will influence your system requirements. A larger agency with numerous patients and staff will need a robust system capable of handling high volumes of data and user activity. Conversely, a smaller agency may opt for a more streamlined and affordable system.
- Budget: Determine your budget constraints for the EMR system. Consider the initial purchase cost, ongoing maintenance fees, and any additional costs associated with training, data migration, and ongoing support.
- Specific Needs: Identify the specific needs of your agency, such as patient demographics, care plans, documentation requirements, and reporting functionalities. The EMR system should cater to these specific needs to optimize workflow and improve patient care.
- Desired Functionalities: Define the essential functionalities you require in an EMR system. This may include electronic health records (EHRs), patient scheduling, billing and coding, communication tools, reporting dashboards, and integration with other healthcare systems.
- User-friendliness: Choose a system with an intuitive interface and user-friendly design. This will facilitate staff adoption, minimize training time, and enhance overall system usability.
- Security and Compliance: Ensure the EMR system meets industry standards for data security and HIPAA compliance. This is crucial for protecting patient information and adhering to legal regulations.
- Vendor Support and Training: Evaluate the vendor’s reputation for customer support, training programs, and ongoing assistance. This will ensure you have access to reliable support throughout the implementation and use of the EMR system.
- Scalability and Flexibility: Consider the scalability and flexibility of the EMR system to accommodate future growth and changes in your agency’s needs. The system should be adaptable to evolving patient volumes, staff size, and regulatory requirements.
Comparing Different EMR Systems for Home Health
Numerous EMR systems cater specifically to home health agencies, each offering unique features and functionalities. Comparing different systems based on key criteria can help you identify the best fit for your agency.
- Features and Functionalities: Analyze the features and functionalities offered by each system, such as EHR capabilities, scheduling tools, billing and coding options, reporting dashboards, and communication features. Compare the system’s strengths and weaknesses in relation to your agency’s specific needs and desired functionalities.
- Pricing and Cost Structure: Evaluate the pricing models and cost structure of different EMR systems. Consider the initial purchase cost, ongoing maintenance fees, and any additional costs associated with training, data migration, and support. Compare the cost-effectiveness of each system based on your agency’s budget and long-term financial considerations.
- User Reviews and Testimonials: Research user reviews and testimonials from other home health agencies that have implemented the EMR systems you are considering. This can provide valuable insights into the system’s usability, performance, and overall satisfaction levels. Look for reviews that highlight the system’s strengths and weaknesses based on your agency’s specific needs.
- Vendor Reputation and Support: Evaluate the vendor’s reputation for reliability, customer support, and training programs. Research their track record of providing timely and effective support to their clients. Consider the vendor’s commitment to ongoing system updates and enhancements to ensure the system remains relevant and secure in the long term.
- Integration with Other Systems: Assess the system’s ability to integrate with other healthcare systems, such as electronic prescribing platforms, patient portals, and billing software. Ensure seamless data flow between systems to optimize workflow and minimize manual data entry.
Implementing an EMR System in a Home Health Agency
Once you have chosen the right EMR system, a smooth implementation process is essential for maximizing its benefits and minimizing disruption to your agency’s operations. Here’s a step-by-step guide to implementing an EMR system in your home health agency:
- Planning and Preparation: Start with a comprehensive planning phase to define your goals, objectives, and implementation timeline. Establish a dedicated implementation team with representatives from key departments, including IT, clinical staff, and administration. Develop a clear communication plan to keep staff informed throughout the implementation process.
- Training and Education: Provide comprehensive training to all staff members who will be using the EMR system. Tailor the training to individual roles and responsibilities, ensuring staff understand the system’s functionalities and how to use it effectively. Offer ongoing support and resources to address any questions or challenges encountered during the training process.
- Data Migration: Carefully plan and execute the data migration process to transfer existing patient data into the new EMR system. Ensure data integrity and accuracy during the migration process to avoid errors and ensure a seamless transition. Consider working with the EMR vendor or a data migration specialist to ensure a smooth and efficient data transfer.
- Go-Live and Post-Implementation Support: Develop a go-live strategy to minimize disruption to patient care and agency operations. Provide ongoing support to staff during the initial weeks and months after go-live to address any issues or challenges. Regularly monitor system performance and identify areas for improvement to optimize the system’s utilization and effectiveness.
Array
The landscape of home health EMR systems is constantly evolving, driven by advancements in technology and a growing demand for efficient and patient-centric care. This evolution is shaping the future of home health, with emerging trends promising to revolutionize how care is delivered and experienced.
Artificial Intelligence and Predictive Analytics
Artificial intelligence (AI) is poised to transform home health EMR systems by enabling predictive analytics and patient risk assessment. AI algorithms can analyze vast amounts of patient data, including medical history, vital signs, and medication records, to identify patterns and predict potential health issues. This allows healthcare providers to proactively intervene and prevent complications, leading to improved patient outcomes and reduced healthcare costs.
- AI-powered risk assessment tools can identify patients at high risk for readmission or adverse events, allowing for early intervention and personalized care plans.
- Predictive analytics can help anticipate medication needs and potential drug interactions, ensuring optimal medication management for patients.
- AI algorithms can analyze patient data to identify emerging trends and patterns in disease progression, enabling more effective disease management strategies.
Wearable Technology and Mobile Health
Wearable technology and mobile health (mHealth) are revolutionizing patient engagement and remote monitoring in home health. Smartwatches, fitness trackers, and other wearable devices can collect real-time data on vital signs, activity levels, and sleep patterns. This data can be seamlessly integrated with EMR systems, providing healthcare providers with a comprehensive view of the patient’s health status.
- Wearable devices can empower patients to actively participate in their care by tracking their progress and providing valuable insights to their healthcare providers.
- Remote monitoring capabilities allow healthcare providers to track patient vitals and intervene quickly if any issues arise, reducing the need for unnecessary hospital visits.
- Mobile applications can facilitate communication between patients and healthcare providers, enabling easy access to medical records, appointment scheduling, and medication reminders.
Integration with Other Healthcare Technologies
Integrating EMR systems with other healthcare technologies, such as electronic health records (EHRs) and patient portals, is essential for creating a seamless and interconnected healthcare ecosystem. This integration allows for the sharing of patient data across different healthcare settings, improving care coordination and reducing redundancies.
- Integration with EHRs enables healthcare providers to access a comprehensive view of the patient’s medical history, regardless of where they received care.
- Patient portals provide patients with secure access to their medical records, appointment information, and medication instructions, empowering them to actively participate in their care.
- Integration with other healthcare technologies facilitates data exchange and collaboration among healthcare providers, leading to more efficient and effective care delivery.
As the healthcare landscape continues to evolve, EMR systems for home health are poised to play an even more pivotal role. The adoption of advanced technologies, such as artificial intelligence and wearable devices, will further enhance patient engagement, streamline data analysis, and drive innovation in home health. By embracing these advancements, home health agencies can create a future where patient-centered care is delivered with greater efficiency, precision, and compassion.
Question Bank
What are the key benefits of implementing an EMR system in a home health agency?
EMR systems offer numerous benefits for home health agencies, including improved patient care through better communication and reduced medication errors, increased operational efficiency through streamlined workflows and automated tasks, and enhanced regulatory compliance by ensuring adherence to industry standards.
How can I choose the right EMR system for my home health agency?
Selecting the right EMR system involves considering factors such as your agency’s size, budget, specific needs, and desired functionalities. It’s crucial to compare and contrast different systems based on key criteria like user-friendliness, data security, and integration capabilities.
What are the potential challenges of implementing an EMR system in a home health agency?
Implementing an EMR system can present challenges, including the need for staff training, data migration, and ensuring a smooth transition. It’s important to have a well-defined implementation plan and provide adequate support to staff during the process.